Combat thermal damage

Thermal injuries fall into two obvious types: burns and frostbite. If everyone has experienced frostbite and hypothermia of varying severity in one way or another, then a serious burn in our lives is not such a frequent guest.
During the Great Patriotic War, burns accounted for 1–2% of sanitary losses. During the arms race, the emergence of nuclear and incendiary weapons, the probability of such losses has increased many times over. Burns from aviation napalm during the Korean War accounted for 25%, and in Vietnam - 45% of the number of sanitary losses. During armed conflicts in the North Caucasus, the frequency of burns reached 5%. At the same time, the frequency of cold injury during combat operations in winter can reach 5–35%.
Classification
A systematic study of thermal lesions in our country began in the 1930s at the Institute of Experimental Surgery in Moscow (A.V. Vishnevsky) and at the Leningrad Institute of Emergency Medicine (I.I. Dzhanelidze). Cold injury was studied at the Military Medical Academy (S. S. Girgolav). In 1960, in the Navy Medical Academy. S. M. Kirov, the first department of thermal injuries was opened, headed by T. Ya. Ariev. Modern principles for the treatment of thermal injuries, taking into account the experience of local wars, were developed by V. A. Dolinin, B. S. Vikhriev.
The classification of burns is based on the depth of damage to the skin and other tissues. There are four degrees:
1. Hyperemia (redness from overflow of blood vessels) and swelling of the skin.
2. Formation of bubbles.
3. Complete or incomplete necrosis of the entire thickness of the skin.
4. The necrosis of the skin and tissues located under the deep fascia (a layer of dense connective tissue that may surround individual muscles or their groups);
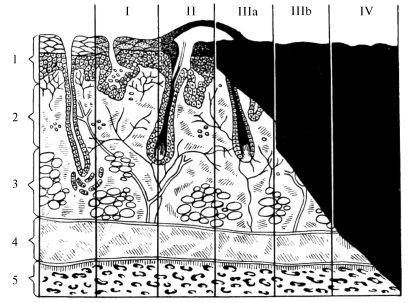
Classification of burns by degree depending on the depth of tissue damage; vertically: 1 - epidermis, 2 - dermis, 3 - subcutaneous fat layer, 4 - muscles, 5 - bone; horizontally - Roman numerals indicate the degree of burn, black - the depth of the lesion.
If many of us have encountered first and second degree burns in everyday life and know that they are unpleasant, but they heal quite successfully, then starting with third degree burns, the body begins to have difficulties.
With a severe burn of the third degree, complete death of the skin, sweat and sebaceous glands, hair follicles occurs, and the subcutaneous tissue is also damaged. Such a wound heals on its own for a very long time and only if it is small. Fourth degree burns don't heal on their own. To restore the skin with such lesions is possible only by surgery in specialized hospitals.
In addition to the degree of burn, its total area is of great importance. There are a number of methods and schemes for determining the area of the burn surface, for example, the rule of nines and the rule of the palm.
The "Rule of nines" is based on equating the area of individual parts of the adult body to a value of 9%. Thus, the head and neck form 9%, the front and back surface of the body - 36% (18% per side), upper limbs - 18% (9% per arm), lower - 36% (18% per leg) .
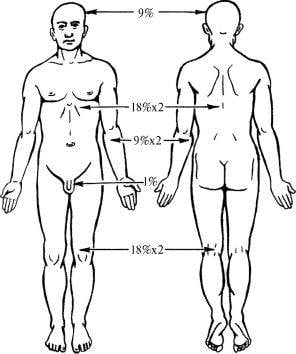
The “rule of the palm” is based on the ratio of the area of the palm to the entire surface of the body, which gives 1-1,2%. This method is used to determine the area of small burns or multiple lesions, including those located on different parts of the body.
With superficial burns of 20–30% and deep burns of more than 10% of the body surface, a burn disease develops. This is a set of pathological processes, among which the leading role belongs to endotoxicosis (poisoning by products of impaired metabolism). A variety of pathological changes in internal organs and system disorders are secondary problems.
There are four periods of burn disease:
1. Burn shock. Manifested by hypovolemia (an abnormally low level of intracellular fluid in the body), disorders of microcirculation, hemodynamics, water-electrolyte and acid-base balance, kidney function, gastrointestinal tract and disorders of the psycho-emotional sphere.
2. Acute burn toxemia. Intoxication of the body with bacterial toxins, protein breakdown products, as well as substances of the paranecratic zone. In addition, neuropsychiatric disorders are characteristic: psychomotor agitation, delirium, insomnia or, conversely, drowsiness, as well as high fever, dyspeptic disorders.
3. Septicotoxemia. Infectious complication associated with scab rejection.
4. Recovery.
In addition to damage to the skin, there are also thermal inhalation lesions that occur during fires in confined spaces, military equipment and in the centers of the use of combat fire mixtures. A few hours after the burn of the respiratory organs, there may be a pronounced edema of the oral mucosa and subglottic space with the development of stenotic asphyxia.
There are burns of the upper respiratory tract, spreading from the mucous membrane of the lips and anterior nasal passages to the larynx, and thermochemical damage to the respiratory tract by combustion products (most often carbon and nitrogen compounds), extending to the entire respiratory tract. Both forms of damage, depending on the circumstances of the injury, can occur in isolation, but more often they are combined. A feature of thermal lesions of the respiratory tract is the toxic effect of soot particles that settle on the mucous membrane of the trachea and bronchi and cause inflammation and even necrosis of epithelial cells.
Burn shock is especially difficult for victims of napalm. In the second and third periods of burn disease, they develop severe intoxication, burn cachexia. Rejection of necrotic tissues is slow, infectious processes in the burn wound are difficult, secondary anemia is rapidly growing, and the function of the endocrine glands is impaired. After healing of napalm burns, disfiguring keloid scars remain.
First aid
First of all, it is necessary to remove the victim from the outbreak. Next, you need to remove the smoldering and burnt clothes, but in no case tear off the fragments of clothing that have stuck to the burnt surface. It is allowed to cut them, if possible.
For minor burns, a PPI bandage or a special agent is applied, for example, it is recommended to use the Apollo anti-burn bandage that has become actively used. No, this is not advertising, it’s just that this tool is now preferred, and I don’t see the point in pointing out something else. Such a bandage is used for burns of 2-3 degrees and has a beneficial effect on the development of a burn disease. The bandage is made of a textile fabric coated with a hydrogel containing an anesthetic and an antiseptic. The bandage was developed jointly with the Russian Institute of Surgery. A. V. Vishnevsky.
For extensive burns, any dry, clean cloth that does not contain ointments or fats can be used as a bandage. In case of burns of the extremities, accompanied by bone fractures, transport immobilization is necessary.
The main attention at the stage of first aid is given to the prevention and elimination of life-threatening conditions. According to indications, analgesics, respiratory and cardiac agents are administered, oxygen is inhaled. Thirst quenching, compensation for fluid and electrolyte losses are carried out by drinking an alkaline-salt solution (1 teaspoon of table salt and 1/2 teaspoon of baking soda per 1 liter of water).
Specialized medical care for burns in a large-scale war is provided in specialized burn hospitals (VPOzhG), burn departments of multidisciplinary (VPMG) or general surgical hospitals (VPKhG) of hospital bases, in hospitals for the lightly wounded (VPGLR).
Rehabilitation treatment and medical rehabilitation of severely burned patients is carried out in the rear health care hospital.
Conclusions
If you pay attention to the composition of first-aid kits, which are independently completed by volunteers and mobilized, then in most cases there are anti-burn agents. This is due not so much to the fact that everything is collected according to plus or minus one list, but to banal logic.
The risk of getting burns is directly related to the military specialization of a fighter. For example, for the crews of armored vehicles, a special protective kit "Warrior-3K" was adopted, which consists of a bulletproof vest, an armored helmet and overalls that protect against open flame for at least 15 seconds. It is assumed that 15 seconds should be enough to leave the burning equipment. Nevertheless, the description of the kit does not indicate whether it includes an individual first aid kit that would take into account the specifics of working in armored vehicles (at least an anti-burn agent and an oropharyngeal air duct).
I suppose that, at best, the fighters are equipped with a standard individual first-aid kit, which will do little to help with burns, but for technology there is a separate, which you must not forget to capture along with weapons and ammunition at the exit. This whole scheme, it seems to me, does not take into account the fact that a fighter leaves the car not during exercises, but most likely under fire and exposure to mine blast injury.
As a result, some crews, like many specialists from other VUS, are forced to take care of themselves, purchasing burns with their hard-earned money, which hints at some omission in their provision and creates a feeling of ignoring the specifics of the work.
Information